
J Cardiothorac Surg 11(1):122įreedman RJ (1991) The intra-aortic balloon pump system: current roles and future directions.
#Intra aortic balloon pump Pc#
Parissis H, Graham V, Lampridis S, Lau M, Hooks G, Mhandu PC (2016) IABP: history-evolution-pathophysiology-indications: what we need to know. The presence of aneurysms or dissection should not be observed, which are contraindications for the procedure (Fig.

From the ventral face, the celiac trunk emerges first, and then the superior mesenteric artery runs parallel to the aorta, following the aorta to the aortic bifurcation. Ultrasound assessment is performed with the patient in the supine position with a low-frequency (2 to 5 MHz) transducer, in a subxiphoid left paramedian longitudinal section, using the left hepatic lobe as a window, the abdominal aorta is represented as a pulsatile and anechogenic tubular image, supported on the vertebral bodies. When the medical team decides to use IAoBC, the presence of any contraindication for the procedure (aortic valve disease, significant bleeding disorder or infection at the femoral puncture site) should be ruled out, and a clinical evaluation should be performed to rule out severe peripheral artery disease.Īfter explaining the procedure and asking the patient to sign an informed consent form, the IAoBC is inserted. This technique is original, and similar techniques have not been previously described. This article proposes an ultrasound-guided IAoBC insertion technique in the cardiovascular ICU. The use of ultrasound to perform femoral vascular access during the insertion of the IAoBC and the use of transesophageal echocardiography (TEE) for positioning it has been described however, since TEE is an invasive procedure, it is not routinely recommended. The proposed mechanism involves mechanical disruption of the balloon against an atherosclerotic plaque or a calcified aorta and negative pressure created during deflation.

This is very rare and occurs in less than 0.5% of cases. IAoBC rupture is not frequent, but can cause a gas embolism and potential entrapment in the arterial tree. Hematoma incidence ranges from 0.4 to 3.9%, and bleeding incidence ranges from 0.4 to 27.7% (mean 5.27 ± 8.5). Ischemia was resolved in most cases by removing the balloon and in 5.8% by thrombectomy only one patient developed gangrene, which required amputation. showed that slowed pulse and cold feet were detected in 29.5% of the cases. Ischemic vascular complications range from 8 to 18%, with critical lower-limb ischemia lower than 1%. Vascular lesions can be catastrophic and evident during IAoBC insertion however, inadvertent dissection of the aorta or iliac artery can go unnoticed, and such dissection is suspected before death in only 20% of cases. , in abdominal tomographies, found 68.2% disagreement in balloon length related to the distance between the subclavian artery and the celiac trunk, which was associated with abdominal vessel obstruction and worse clinical outcomes. The main complications of using IAoBC result from insertion and malpositioning.

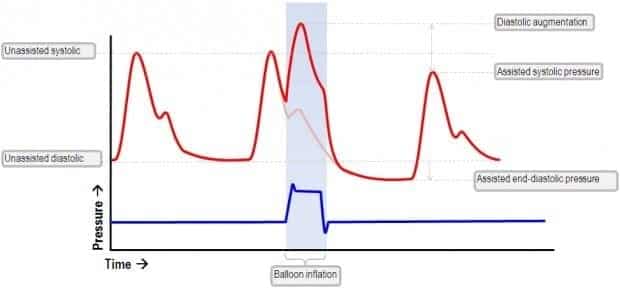
IAoBC has been used in different groups of patients, including in those with cardiogenic shock, regardless of its etiology, refractory angina, acute myocardial infarction, refractory ventricular arrhythmias, mechanical infarct complications (acute mitral regurgitation and ventricular septal rupture), high-risk angioplasty and high-risk cardiac or noncardiac surgery, with different outcomes. Despite the theoretical physiological advantages of IAoBC, its effect on decreasing mortality is controversial. IAoBC is used in this context to support coronary circulation and to reduce stress on the left ventricle. Intra-aortic balloon counterpulsation (IAoBC) is used in up to 7% of cardiac surgery patients.


 0 kommentar(er)
0 kommentar(er)
